SINGAPORE – Women with a family history of cancer should go for DNA testing regardless of age to see if they have mutated hereditary cancer genes, which put them at high risk of getting the disease in the breasts, ovaries, or elsewhere.
Those found to have the mutated genes should go for cancer screening every year, said associate professor of genomic medicine Joanne Ngeow at Nanyang Technological University’s (NTU) Lee Kong Chian School of Medicine.
Men with the mutated genes are also at risk of getting cancer, even in the breasts, she told The Straits Times.
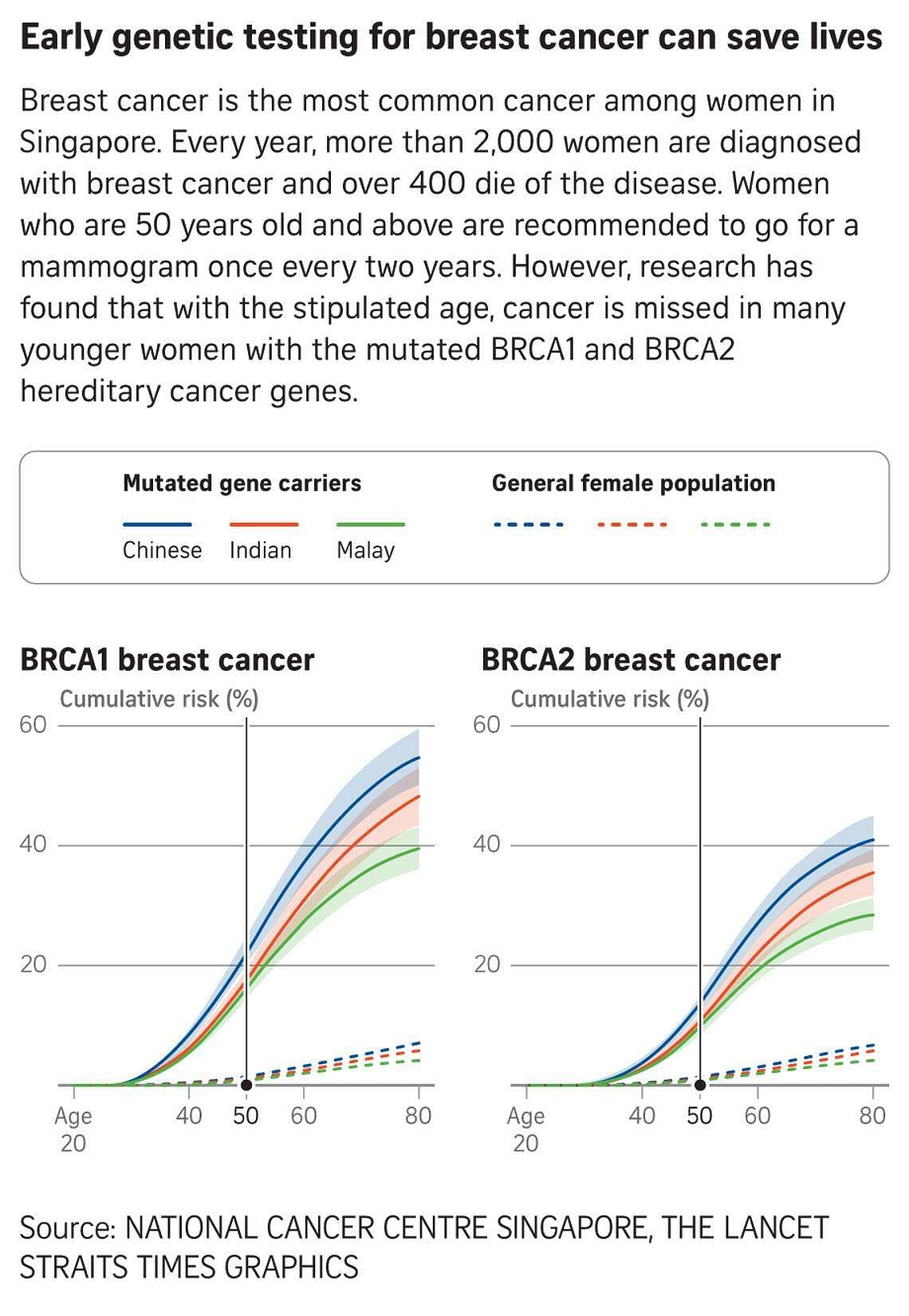
While a mammogram has been an effective method for detecting breast cancer early in women aged 50 and above, there is no recommendation for younger women to go for the test and, as a result, cancer is often missed in younger women with the mutated hereditary cancer genes.
These findings are from a recent study on carriers of mutated cancer genes in Singapore and Malaysia.
It provides an important framework for estimating cancer risks in Asian carriers, allowing a more tailored approach to managing the disease in Singapore.
Breast cancer is the most common cancer among women here. More than 2,000 women are diagnosed with it annually, and more than 400 die from the disease.
The study was conducted by Prof Ngeow and other researchers from institutions such as NTU, National Cancer Centre Singapore (NCCS), Agency for Science, Technology and Research, Cancer Research Malaysia and University of Malaya. The findings were published in The Lancet Regional Health – Western Pacific in February 2024.
All men and women have hereditary cancer genes – breast cancer gene 1 (BRCA1) and breast cancer gene 2 (BRCA2) – which produce proteins to help repair damaged DNA. However, only some have mutations in either of the genes.
The study, the largest so far on an Asian population, involved 572 Asian families in Singapore and Malaysia with the mutated genes.
Family members were between 20 and 79 years old and of Chinese, Indian and Malay ethnicity. Women made up 95 per cent of the group.
About 13 per cent (144) of the 1,121 BRCA1 carriers were diagnosed with breast cancer, while 5.8 per cent (65) had ovarian cancer.
Breast cancer was detected in almost 12 per cent (152) of the 1,275 BRCA2 carriers, and ovarian cancer in 1.5 per cent.
The study has also shown that the estimated risks of breast and ovarian cancers for carriers here are similar to that of Asians in the West.
“We have healthy exposures, unhealthy exposures, healthy genes and unhealthy genes. So how do we use this information to better help us decide who’s likely to stay healthy, who’s likely to get the disease?” said Prof Ngeow, who heads the Cancer Genetics Service at NCCS.
Based on the 2021 Singapore Cancer Registry Annual Report, breast cancer topped the list of cancer cases in women between 2017 and 2021, making up 30 per cent of the total cases. The disease also accounted for 17.3 per cent of cancer deaths – the highest proportion.
Over the same period, cases of ovarian cancer rose to about twice the number in the previous five-year period, ranking sixth in incidence and death for women.
In 2022, a study published under Singapore’s National Precision Medicine Programme listed the entire genetic make-up of 10,000 Singaporean women.
It also looked at hereditary breast-ovarian cancer syndrome, which was what Hollywood megastar Angelina Jolie had.

“We found that one in 150 Singaporeans carries a genetic mutation associated with hereditary breast-ovarian cancer syndrome, putting them at risk. This number is quite high,” Prof Ngeow said.
In 2013, Ms Jolie underwent a prophylactic double mastectomy as a precaution against cancer, as she carried the “faulty gene” that significantly raised her odds. She had inherited the BRCA1 gene from her mother, actress Marcheline Bertrand, who died of ovarian cancer at the age of 56.
Ms Jolie’s doctors estimated she had an 87 per cent risk of developing breast cancer and a 50 per cent risk of ovarian cancer.
Two years after her double mastectomy, Ms Jolie, who is also a UN envoy, underwent surgery to remove her ovaries and fallopian tubes.
Prof Ngeow said carriers of the mutated genes here do not have to take such drastic measures.
Instead, they can go through more frequent surveillance.
“For example, we may start with MRI (magnetic resonance imaging) for the breasts from the age of 30 onwards for patients who are BRCA1 (carriers),” she said. “Also frequent mammograms – not one every two years, but one every year.”
She added: “There are patients who may choose prophylactic double mastectomy, but we do not strongly advocate that.”
As for ovarian cancer, Prof Ngeow admitted that there are no good screening tests available.
“We do recommend that once patients are done with childbearing and close to menopause, to remove the ovaries and fallopian tubes as part of reducing the risks,” she said.
“By doing that, it reduces the risk of ovarian cancer by more than 90 per cent and cuts down breast cancer risk to some degree.”
It is not a foolproof option, as in the case of Madam Elaine Ho, a 64-year-old teacher aide at a special needs school.
She went for genetic testing at NCCS because she has a family history of cancer – her eldest sister was BRCA1 positive and had both breast and ovarian cancers, her other sister died at 59 after her breast cancer relapsed, and even one of her brothers was diagnosed with lung cancer.
Having tested positive for BRCA1 in 2017, Madam Ho agreed to remove her ovaries and fallopian tubes to prevent cancer but opted to go for regular mammograms to retain her breasts.
But she was later diagnosed with cancer in her left breast and was shocked.
“I decided to remove both my breasts and not carry out reconstruction. My chemotherapy sessions were not easy. I was bloated. I had nausea and vomiting. My husband was my rock. He and my daughters were by my side all the way,” she said.
Madam Ho added that while her daughters tested negative, her brothers refused to get tested for the mutated genes.
Prof Ngeow said: “It is understandable, as BRCA stands for ‘breast cancer gene’.”
But she noted: “BRCA gene mutations are associated with multiple cancer types and aren’t limited to women. Men with BRCA1 and BRCA2 mutations are at increased risk of breast, prostate, pancreatic and other types of cancers, and should also consider getting tested.”


